Thalassemia Treatment Cost in India
Thalassemia is a severe genetic blood disorder that requires timely and ongoing medical care, often involving blood transfusions and potentially a bone marrow transplant for a cure. For international patients seeking effective treatment at a reasonable price, India has become a leading destination for medical care. The cost of thalassemia treatment in India ranges from as low as $1,200 for routine care to $35,000 for a bone marrow transplant, depending on the severity of the condition, the type of treatment, and the patient's specific needs. Compared to countries like the USA, the UK, or Thailand, India offers high-quality care at nearly one-third the cost, with advanced medical infrastructure, internationally trained doctors, and comprehensive support services for foreign patients.
What is Thalassemia?
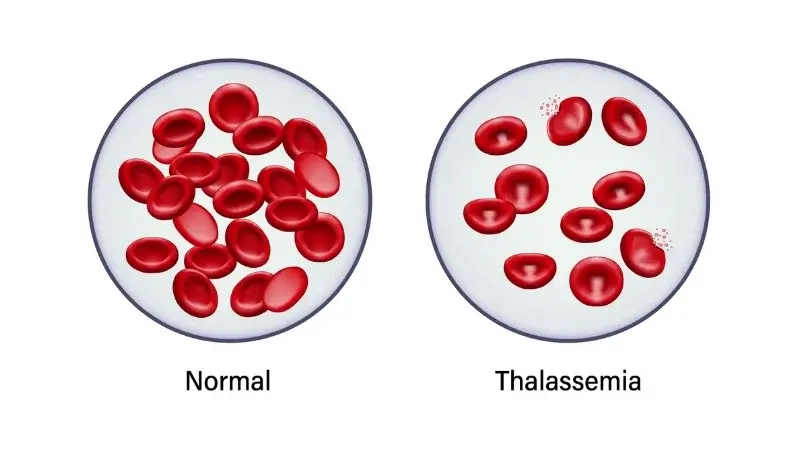
Thalassemia is a genetic blood disorder that affects the body's ability to produce normal hemoglobin. Hemoglobin is the protein found in red blood cells responsible for carrying oxygen throughout the body. In individuals with thalassemia, the production of hemoglobin is either reduced or abnormal, resulting in anemia, a condition characterized by fatigue, weakness, and pale skin.
Thalassemia disorder is inherited, meaning it is passed down from parents to their children through mutated genes. Thalassemia is more prevalent in individuals from Mediterranean regions, South Asia, the Middle East, and certain parts of Africa. The condition can range from mild, causing few or no symptoms, to severe, requiring regular medical treatment to manage complications.
Thalassemia leads to a shortage of healthy red blood cells in the body. Without enough red blood cells, oxygen delivery to organs and tissues becomes impaired. Over time, this can result in serious health problems such as delayed growth, bone deformities, iron overload from repeated transfusions, and organ damage.
While thalassemia is a lifelong condition, modern medical treatments have significantly improved its management and treatment outcomes. With proper care (especially from experienced doctors), patients can live active and fulfilling lives. In some cases, a bone marrow transplant can offer a potential cure.
What are the Different Types of Thalassemia?
Thalassemia is classified based on which part of the hemoglobin molecule is affected, either the alpha or beta globin chains. The number and type of gene mutations determine the severity of the condition. Here are the main types:
- Alpha Thalassemia: Alpha thalassemia occurs when there is a mutation or deletion in one or more of the four alpha-globin genes. The severity increases with the number of affected genes:
- Silent Carrier (1 gene affected): Typically, no symptoms. The person is a carrier and may pass the gene to their children.
- Alpha Thalassemia Trait (2 genes affected): Causes mild anemia but usually doesn't require treatment.
- Hemoglobin H Disease (3 genes affected): Leads to moderate to severe anemia, enlarged spleen, and may need occasional transfusions.
- Alpha Thalassemia Major (4 genes affected): Also known as hydrops fetalis, this is the most severe form and often leads to stillbirth or death shortly after birth without intervention.
- Beta Thalassemia: Beta thalassemia occurs when mutations affect the beta-globin gene. There are three main subtypes:
- Beta Thalassemia Minor (Trait): Only one gene is mutated. The person may have mild anemia or no symptoms. No treatment is typically required, but genetic counseling is essential for future family planning.
- Beta Thalassemia Intermedia: Both beta-globin genes are affected, but the mutations are less severe. Patients may have moderate anemia and might require occasional blood transfusions, especially during illness or stress.
- Beta Thalassemia Major (Cooley's Anemia): This is the most severe form, characterized by severe mutations in both genes. Symptoms appear in the first two years of life and include severe anemia, poor growth, bone deformities, and fatigue. Lifelong blood transfusions are necessary, and a bone marrow transplant is the only potential cure.
- Other Rare Forms: Some rare variants include:
- E-beta Thalassemia: A combination of beta-thalassemia and hemoglobin E disease, commonly found in Southeast Asia.
- Doubly Heterozygous States: Where mutations affect both alpha and beta genes or other hemoglobin-related abnormalities.
What are the Symptoms of Thalassemia?
The symptoms of thalassemia vary greatly depending on the severity of the condition. Some individuals may be carriers and never experience any symptoms. Others, especially those with severe forms, such as thalassemia major, may begin to show signs within the first few months of life.
Below is a detailed overview of the common symptoms observed in thalassemia patients:
General Symptoms of Anemia
Thalassemia causes the body to produce fewer and less effective red blood cells, leading to chronic anemia. This results in:
- Fatigue and weakness even after light activity due to poor oxygen supply.
- Pale or yellowish skin (jaundice) from the breakdown of abnormal red blood cells.
- Shortness of breath, especially during exertion.
- Dizziness or light-headedness, particularly when standing up quickly.
- Cold hands and feet are caused by reduced circulation.
Symptoms in Children and Infants
In moderate to severe cases, symptoms typically begin to appear between 3 to 6 months of age and may include:
- Irritability or fussiness, often due to fatigue or discomfort.
- Poor appetite and difficulty feeding.
- Delayed growth and development, such as late milestones or poor weight gain.
- Frequent infections due to a weakened immune system.
- Failure to thrive, especially in infants with thalassemia major.
Bone-Related Changes
In chronic cases, the body attempts to compensate for the lack of red blood cells by expanding the bone marrow. It leads to:
- Bone deformities, especially in the face and skull.
- Frontal bossing is an abnormal protrusion of the forehead.
- Thinning and weakening of bones increases the risk of fractures.
Enlarged Organs
Ongoing destruction of abnormal red blood cells and iron overload from transfusions can cause:
- An enlarged spleen (splenomegaly) can cause abdominal fullness and increase the risk of infection or bleeding.
- Liver enlargement (hepatomegaly), potentially affecting digestion and metabolism.
Iron Overload Symptoms
Patients who receive frequent blood transfusions are at risk of iron overload, a serious condition that can damage vital organs. Symptoms may include:
- Joint pain and stiffness due to iron deposits.
- Darkening of the skin, often referred to as "bronze diabetes."
- Heart problems, such as arrhythmias or heart failure.
- Diabetes or other hormonal issues are caused by damage to the pancreas or endocrine glands.
Psychological and Social Effects
Living with thalassemia can also lead to emotional and mental health challenges:
- Low self-esteem, especially in children with physical changes or frequent hospital visits.
- Depression or anxiety is due to the chronic nature of the disease.
- Social withdrawal or academic struggles caused by fatigue or absenteeism from school.
When to Seek Medical Attention: Early diagnosis and management are crucial for effective treatment. If a child exhibits persistent fatigue, pale skin, or failure to grow normally, prompt medical attention should be sought. Proper evaluation can lead to early treatment and a significantly better quality of life.
How is Thalassemia Diagnosed?
Early and accurate diagnosis of thalassemia is crucial for managing the disease effectively and planning long-term treatment. In India, hospitals use advanced diagnostic tools to not only confirm the presence of thalassemia but also to determine its type and severity. It enables doctors to create personalized treatment plans that enhance outcomes and minimize complications.
Medical History and Physical Examination
The diagnostic process begins with a thorough medical history and a comprehensive physical examination. Doctors will look for signs such as:
- Chronic fatigue, pale or yellowish skin, and shortness of breath.
- Family history of anemia or blood disorders.
- Signs of delayed growth or bone deformities in children.
- An enlarged spleen or liver during a physical exam.
While these signs can suggest anemia, further lab tests are required to confirm thalassemia.
Complete Blood Count (CBC)
A CBC test is the first lab investigation. It measures various components of the blood, such as:
- Hemoglobin levels are typically low in thalassemia.
- The red blood cell (RBC) count is often lower, or the cells are abnormally shaped.
- Mean corpuscular volume (MCV) is usually reduced in thalassemia.
Low hemoglobin and MCV values raise suspicion of thalassemia but are not conclusive.
Peripheral Blood Smear
In this test, a blood sample is viewed under a microscope. Typical findings in thalassemia include:
- Abnormally small (microcytic) and pale (hypochromic) red blood cells.
- Irregular shapes or target cells.
- Nucleated red blood cells are found in severe cases.
This test helps differentiate thalassemia from other causes of anemia, like iron deficiency.
Hemoglobin Electrophoresis
Hemoglobin electrophoresis is a definitive test for diagnosing thalassemia. It separates the different types of hemoglobin in the blood:
- Increased levels of Hemoglobin F (fetal hemoglobin) and Hemoglobin A2 often indicate beta-thalassemia.
- It helps distinguish between beta thalassemia minor, intermedia, and major.
The test may not detect some forms of alpha thalassemia, so further genetic testing may be necessary.
High-Performance Liquid Chromatography (HPLC)
HPLC is an advanced version of hemoglobin analysis. Many hospitals use HPLC for its:
- Higher accuracy in identifying abnormal hemoglobin variants.
- Ability to monitor changes in hemoglobin levels over time.
Genetic Testing
DNA analysis is used to confirm mutations in alpha or beta globin genes. It is beneficial for:
- Prenatal diagnosis to detect thalassemia in unborn babies.
- Determining if both parents are carriers.
- Differentiating between similar blood disorders.
Genetic testing is essential for planning bone marrow transplants and for couples considering children.
Iron Studies
These tests are used to rule out iron deficiency anemia, which shares similar symptoms with thalassemia. Tests include:
- Serum ferritin
- Total iron-binding capacity (TIBC)
- Transferrin saturation
Prenatal Screening
In families with a history of thalassemia, prenatal screening can be performed using:
- Chorionic villus sampling (CVS) at 10–12 weeks.
- Amniocentesis at 15–20 weeks.
Prenatal screening helps identify if the fetus has inherited severe forms of thalassemia.
How is Thalassemia Treated in India?
India has become a global hub for thalassemia treatment, offering care that ranges from regular blood transfusions to curative bone marrow transplants. Treatment protocols follow international standards, ensuring safe, effective, and personalized care for each patient.
Blood Transfusions
Regular red blood cell transfusions are the primary treatment for moderate to severe thalassemia, especially for patients with thalassemia major. These transfusions:
- Replenish healthy red blood cells and hemoglobin levels.
- Help manage symptoms like fatigue, poor appetite, and delayed growth.
- They are typically required every 2 to 4 weeks, depending on the patient's condition.
Indian hospitals provide safe, screened blood with high standards for infection control and compatibility.
Iron Chelation Therapy
Frequent transfusions lead to iron overload, which can damage the heart, liver, and endocrine glands. To remove excess iron, patients are given iron-chelating drugs such as:
- Deferoxamine (Desferal): An injectable drug used several times a week.
- Deferasirox (Exjade, Jadenu): An oral tablet taken daily.
- Deferiprone (Ferriprox): Another oral option, often used in combination with other chelators.
These drugs are available at affordable prices in India, and treatment is monitored closely by hematology specialists.
Folic Acid Supplements
Patients are often prescribed folic acid to support the production of red blood cells. While it doesn't replace other treatments, it helps improve energy levels and overall blood health.
Bone Marrow Transplant (BMT)/Stem Cell Transplant
A bone marrow transplant is currently the only curative treatment for thalassemia, especially in children with thalassemia major. In India, BMT is offered at world-class centers, such as the Fortis Memorial Research Institute (FMRI) in Gurgaon, under the care of renowned doctors like Dr. Rahul Bhargava.
The process includes:
- High-dose chemotherapy is used to destroy faulty bone marrow.
- Infusion of healthy stem cells from a compatible donor (usually a sibling).
- Close monitoring in sterile isolation units for infection control.
India has one of the highest BMT success rates globally for pediatric thalassemia patients, especially when done early in life.
Gene Therapy (Emerging Treatment)
Gene therapy aims to correct the genetic defect causing thalassemia. While still in the research and limited clinical use phase, India is expected to introduce more accessible gene therapy options in the coming years at a fraction of global costs.
Supportive Care
Patients also receive:
- Vaccinations and antibiotics to prevent infections, especially if the spleen is removed.
- Hormone replacement therapy is used if endocrine functions are affected.
- Psychological counseling to support mental health and quality of life.
What is the Cost of Thalassemia Treatment in India?
One of the significant reasons international patients choose India for thalassemia care is the affordable and transparent pricing. India offers high-quality treatment at a fraction of the cost compared to countries like the United States, the United Kingdom, or Germany without compromising on medical standards, safety, or patient outcomes.
The cost of thalassemia treatment in India ranges from $1,200 to $35,000, depending on the type and severity of the condition and the specific treatment required (transfusion-based care vs. bone marrow transplant).
- Cost of Regular Blood Transfusions: The cost of regular blood transfusions in India typically ranges from $150 to $2 per session, depending on the hospital and patient requirements. On average, thalassemia patients requiring monthly transfusions spend around $1,200 to $2,500 per year on transfusion-related care, including pre-transfusion testing and administration charges.
- Cost of Iron Chelation Therapy: In India, iron chelation therapy, which is essential for managing iron overload resulting from repeated transfusions, costs between $300 and $1,000 per month, depending on the specific medication used (Deferasirox, Deferiprone, or Desferal).
- Cost of Supportive Care: Patients with moderate thalassemia may require supportive medications such as folic acid and antibiotics, with an estimated annual cost of $300 to $800.
- Cost of Bone Marrow Transplant (BMT) in India: For those pursuing a cure, the bone marrow transplant cost in India for thalassemia ranges between $24,000 and $28,000 for a matched sibling donor. If a haploidentical (half-matched) transplant is required, the treatment cost increases to approximately $28,000 to $32,000 due to additional pre-transplant conditioning and post-transplant care. Unrelated donor transplants, which are rare and complex, can cost up to $45,000, inclusive of donor matching, stem cell procurement, and prolonged hospitalization.
What are the Factors Affecting Thalassemia Treatment Costs in India?
The total cost of thalassemia treatment in India can vary from patient to patient. Several medical and logistical factors influence the overall expenditure. Understanding these factors helps international patients and their families make informed decisions and prepare better financially for their treatment journey.
- The type and severity of thalassemia have a significant impact on the overall treatment cost in India. Patients with thalassemia major often require lifelong blood transfusions and chelation therapy. At the same time, those eligible for a bone marrow transplant may face higher upfront costs with a potential long-term cure.
- The choice of treatment modality plays a key role in determining cost. Regular transfusions are less expensive in the short term, but curative options like a bone marrow transplant, while more costly initially, may reduce long-term medical expenses.
- The cost of thalassemia treatment in India is also influenced by the hospital and city selected. Premium multispecialty hospitals in cities like Delhi, Mumbai, Bangalore, or Gurgaon may charge more than mid-tier hospitals in smaller towns, but they offer international accreditations and advanced transplant facilities.
- The type of bone marrow donor available impacts the transplant cost. A matched sibling donor transplant is the most cost-effective, while a haploidentical or unrelated donor transplant increases the price due to complex matching procedures and higher complication risks.
- Patient age and weight are essential cost determinants. Pediatric patients often require different drug dosages, monitoring schedules, and ICU support, which can slightly alter the total cost of thalassemia care in India.
- Post-treatment recovery and follow-up care can increase the overall cost of care. Bone marrow transplant patients need regular follow-ups, medications to prevent graft-versus-host disease (GVHD), and nutritional support, especially in the first six months post-surgery.
- Complications or co-existing health conditions may increase the cost of thalassemia treatment. Conditions such as liver enlargement, spleen disorders, infections, or heart problems can result in additional diagnostic tests, medications, or ICU stays.
- The duration of the hospital stay is another variable factor. While standard BMT hospitalizations typically range from 3 to 4 weeks, complications can extend the stay and increase associated costs, including room charges, nursing care, and isolation protocols.
- The need for iron chelation therapy adds to long-term costs. Patients undergoing regular transfusions often spend thousands of dollars annually on iron chelators to prevent organ damage, especially if not undergoing a transplant.
Thalassemia Treatment Cost Comparison: India vs. Other Countries
When it comes to managing a chronic condition like thalassemia, cost plays a significant role in decision-making, especially for international patients. One of the most considerable advantages India offers is world-class thalassemia treatment at a much lower price compared to many Western and Southeast Asian countries. Patients from the United States, the United Kingdom, Africa, and the Middle East often travel to India to access the same level of medical care at up to 80% lower prices.
- In India, the cost of bone marrow transplants for thalassemia starts at $24,000. In contrast, the same procedure can cost upwards of $150,000 in the United States, making it nearly six times more affordable in India.
- Iron chelation therapy in India costs approximately $4,000 to $10,000 per year, depending on the specific drug and dosage. In contrast, the same treatment in the UK or USA can cost over $25,000 per year, significantly increasing long-term expenses for transfusion-dependent patients.
- Blood transfusions in India cost approximately $150 to $250 per session, totaling $1,200 to $2,500 annually, whereas the same transfusion regimen in Western countries can cost between $15,000 and $20,000 per year.
- Supportive care costs, including folic acid, hormone therapy, antibiotics, and diagnostics, remain under $800 annually in India, compared to several thousand dollars in countries with high healthcare costs.
- Hospitalization and medical consultation fees in India are substantially lower than in many other countries. Even at premium centers like the Fortis Memorial Research Institute (FMRI), patients benefit from international-standard care at a fraction of the cost it would incur in European or North American facilities.
Cost Comparison Table
|
Country |
Bone Marrow Transplant Cost |
Iron Chelation Therapy (Yearly) |
Blood Transfusion Cost (Yearly) |
|
India |
$25,000 – $35,000 |
$4,000 – $10,000 |
$1,200 – $2,500 |
|
USA |
$150,000 – $250,000 |
$25,000 – $30,000+ |
$15,000 – $20,000+ |
|
UK |
$120,000 – $180,000 |
$20,000 – $25,000+ |
$12,000 – $18,000+ |
|
Thailand |
$50,000 – $70,000 |
$8,000 – $12,000 |
$3,500 – $5,000 |
|
Germany |
$130,000 – $200,000 |
$25,000+ |
$14,000 – $19,000 |
|
Turkey |
$40,000 – $60,000 |
$10,000 – $15,000 |
$4,000 – $6,000 |
Quality of Thalassemia Treatment in India
India has established itself as a global leader in treating complex blood disorders, such as thalassemia, offering not only cost-effective care but also world-class medical standards. The quality of thalassemia treatment in India is upheld by cutting-edge infrastructure, internationally trained hematologists, advanced transplant facilities, and comprehensive patient support systems. These factors combine to offer foreign patients safe, reliable, and successful treatment options.
- Indian hospitals adhere to international treatment protocols for thalassemia, including those recommended by the World Health Organization (WHO), the American Society of Hematology (ASH), and the European Society for Blood and Marrow Transplantation (EBMT).
- Many hospitals, such as Fortis Memorial Research Institute (FMRI) in Gurgaon, are NABH- and JCI-accredited, indicating that they meet the highest global standards for patient safety, quality of care, and infrastructure.
- Doctors specializing in thalassemia treatment in India are often internationally trained, with vast experience in managing pediatric and adult thalassemia, performing bone marrow transplants, and handling complex cases.
- State-of-the-art bone marrow transplant centers in India feature HEPA-filtered rooms, high-end ICU care, dedicated isolation wards, and on-site transfusion units, minimizing infection risks and enhancing recovery.
- Advanced diagnostic facilities in India offer in-house genetic testing, HLA typing, hemoglobin electrophoresis, and pre-transplant workups, resulting in faster diagnosis and more personalized treatment plans.
- High success rates for bone marrow transplants in India have made the country a trusted option for thalassemia. For matched sibling donor transplants in pediatric patients, survival rates exceed 85% at top centers.
- Indian hospitals offer integrated care, where patients have access to specialists such as hematologists, pediatricians, nutritionists, psychologists, and transplant coordinators, all under one roof, ensuring comprehensive treatment.
- Post-treatment monitoring and follow-up care are well-structured in India, with regular check-ups, liver and cardiac assessments, iron monitoring, and GVHD management provided at affordable prices.
- Patient safety is a top priority, with rigorous infection control protocols, safe blood handling practices, sterile transfusion procedures, and 24/7 emergency care in tertiary hospitals.
- Digital health records, telemedicine support, and international help desks facilitate easier access to follow-up care, the submission of medical reports, and consultations with doctors from their home countries for overseas patients.
Why Global Patients Trust India
- High-quality, ethical care backed by years of clinical excellence.
- Transparent pricing with no hidden costs.
- Personalized treatment plans for each stage of thalassemia.
- Shorter waiting periods compared to Western countries.
- Empathetic medical teams that are trained to work with children and families.
- Proven success stories of patients from Africa, the Middle East, Southeast Asia, and Europe.
What are the Services Available for International Patients Seeking Thalassemia Treatment in India
India has become a preferred medical tourism destination, not just because of its affordable prices and expert doctors but also because of the comprehensive support system it offers international patients. Families traveling from abroad for thalassemia treatment in India can expect seamless coordination, language assistance, and end-to-end care from arrival to recovery.
Here's how India supports international patients every step of the way:
- Dedicated international patient departments in hospitals like Fortis Memorial Research Institute (FMRI), Gurgaon, provide personalized care planning, from the initial medical opinion to hospital discharge.
- Pre-arrival medical consultations are offered via email or video calls, allowing patients to share reports and receive estimated treatment plans, cost breakdowns, and timelines before booking a trip.
- Visa assistance is available through hospital concierge teams, including help with Medical Visa Invitation Letters (MVIL), guidance on documents, and embassy liaison support.
- Airport pickup and drop-off services are arranged for international patients, ensuring a stress-free arrival experience from the moment they land in India.
- Translators and multilingual staff are available in major hospitals to assist patients and their families who speak Arabic, French, Russian, Swahili, Bengali, and other languages.
- Affordable accommodation options are provided near hospitals, ranging from guesthouses and serviced apartments to hotel tie-ups, suitable for both short-term and long-term stays.
- Foreign exchange support and SIM card assistance are available upon arrival, ensuring smooth and convenient communication and financial transactions.
- Dietary preferences and religious needs are respected, with customizable meals tailored to patients' and families' cultural and health requirements.
- Daily updates and progress reports are shared with families, particularly in transplant cases, to ensure complete transparency and involvement in the care process.
- Post-treatment follow-up care is made accessible through teleconsultations, allowing patients to continue their recovery and check-ins without needing to return immediately.
- Medical documentation and treatment summaries are provided in English, along with scans, blood reports, and prescriptions, to ensure continuity of care in the home country.
What is the Success Rate of Thalassemia Treatment in India?
India has achieved remarkable progress in the management and cure of thalassemia, with high success rates across various treatment modalities, especially bone marrow transplants.
- The success rate of bone marrow transplant for thalassemia in India ranges from 80% to 90%, especially in children with thalassemia major who receive a transplant from a fully matched sibling donor.
- Matched sibling donor transplants (MSDT) yield the highest success rates, with top hospitals, such as Fortis Memorial Research Institute in Gurgaon, achieving survival rates above 85% in young patients.
- Haploidentical or half-matched donor transplants, which are performed when a matched sibling is unavailable, have improved over the years with the introduction of new conditioning regimens, offering success rates of 70% to 80% in leading Indian centers.
- Survival rates for blood transfusion and iron chelation-based management are also encouraging, especially when started early and followed consistently. Many patients lead near-normal lives into adulthood with appropriate monitoring.
- Post-transplant recovery outcomes in India are on par with international benchmarks, with most pediatric patients resuming normal activities and education within 6 to 12 months after a successful transplant.
- Low post-transplant infection rates and graft rejection incidences in Indian hospitals are attributed to HEPA-filtered isolation rooms, strong infection control measures, and expert post-op monitoring.
- Indian doctors are known for their expertise in high-risk and second-attempt transplants, which further increases hope for patients who may have had complications or failed procedures elsewhere.
- Long-term follow-up care in India ensures that complications such as graft-versus-host disease (GVHD), iron overload, and endocrine issues are promptly and effectively managed, thereby improving overall survival and quality of life.
Patient Testimonials: Thalassemia Treatment Success Stories in India
Real-life experiences from patients around the world offer powerful insight into the effectiveness and compassion of thalassemia treatment in India. These stories reflect not just medical success but also the emotional relief and hope that families experience after receiving world-class care at a fraction of the global cost. Here are a few inspiring testimonials from international families who traveled to India for thalassemia treatment.
Aliya's Journey from Kenya to a Cure
Aliya, a 5-year-old from Nairobi, was diagnosed with thalassemia major at just 8 months old. Her parents were exhausted by the emotional toll and financial burden of regular transfusions. After researching global options, they chose India and connected with Fortis Memorial Research Institute (FMRI), Gurgaon, where Dr. Rahul Bhargava recommended a bone marrow transplant.
Her older brother was a perfect donor match. The transplant was performed successfully, and after a 3-week hospital stay and 3 months of follow-up, Aliya returned home transfusion-free. Today, she attends school regularly and is thriving.
"We couldn't believe we found such advanced care at a price we could afford," said her father. "India gave our daughter a future."
Hossam's Family Finds Hope in India
Hossam, a 10-year-old boy from Egypt, had been receiving monthly transfusions since infancy. With iron overload beginning to affect his liver, his family sought a long-term solution. They consulted several hospitals before deciding on a haploidentical transplant in India.
Though he didn't have a fully matched sibling donor, Dr. Rahul performed a successful half-matched bone marrow transplant.
"We were nervous at first," his mother shared, "but the care team was with us every step. Today, my son plays football again and no longer depends on blood transfusions."
Sarah's Life Without Transfusions – A UAE Success Story
Born in Dubai, Sarah was diagnosed with beta-thalassemia major at two years old. She underwent regular transfusions and iron chelation for nearly a decade. Her family was referred to India for an evaluation. A matched sibling donor transplant was performed at one of India's premier pediatric centers.
"Within six months, Sarah no longer needed transfusions," said her parents. "India didn't just cure her—it restored our peace of mind."
Musa's Affordable Treatment from Nigeria
Musa, age 7, came to India with his uncle after experiencing complications from poor transfusion management in Nigeria. The family could not afford treatment in Europe or the US but found an affordable package in India. Doctors managed his iron overload with proper chelation, optimized his transfusion schedule, and began exploring transplant options.
"Even without the transplant yet, my nephew is already healthier than we've seen him in years. The medical team is thoughtful, thorough, and deeply caring," his uncle said.
Related Videos
Frequently Asked Questions
Yes, thalassemia is curable in many cases through a bone marrow transplant (also known as a stem cell transplant). BMT is especially effective in children with thalassemia major when a matched donor is available.
The cost of thalassemia treatment in India ranges from as low as $1,200 for routine care to $35,000 for a bone marrow transplant. The cost of treatment depends on the severity of the condition and the type of treatment chosen.
The hospital stay typically ranges from 3 to 4 weeks, depending on the patient's condition and recovery. An additional stay may be required for pre-transplant evaluation and post-transplant monitoring.
Yes. India is home to internationally accredited hospitals, experienced hematologists, and strict infection control protocols. Hospitals like Fortis Memorial Research Institute in Gurgaon follow global standards and are trusted by patients from over 80 countries.
While bone marrow transplants are most successful in children, adults may also be eligible depending on their health status, disease progression, and donor availability. Consultation with a transplant expert in India is recommended.
Doctors in India conduct HLA testing for siblings or close relatives. If no match is found, they may explore haploidentical (half-matched) or unrelated donor transplants, which are increasingly successful due to advances in transplant medicine.
Yes. Most top hospitals offer dedicated international patient services that assist with visa letters, airport pickup, translation, accommodation, and personalized care coordination before, during, and after treatment.
You can email your medical records and receive a preliminary treatment plan and cost estimate before deciding to travel. It helps with budgeting and preparation.
Yes. All reports, prescriptions, and discharge summaries are provided in English and are widely accepted by doctors and insurance providers globally for follow-up and reimbursement purposes.
Yes. Indian hospitals offer teleconsultation services and remote follow-up to stay in touch after discharge. It ensures continuity of care and facilitates remote management of recovery or medication adjustments.