Acute Lymphocytic Leukemia Treatment in India
Acute Lymphoblastic Leukemia (ALL) is a type of cancer that affects the blood and bone marrow, characterized by the overproduction of immature white blood cells (lymphoblasts). The treatment protocol for ALL typically involves chemotherapy, targeted therapies, and in some cases, stem cell transplantation.
What is Acute Lymphocytic Leukemia?
Acute Lymphocytic Leukemia (ALL), also known as Acute Lymphoblastic Leukemia, is a type of cancer that originates in the bone marrow and quickly spreads to the blood. It primarily affects white blood cells, causing them to proliferate uncontrollably and disrupt the production of normal blood cells. This form of leukemia is most common in children but can also affect adults, with peak incidences in children aged 2-5 years and in adults over 50.
How many Types of Acute Lymphocytic Leukemia (ALL)?
| Type | Subtype / Characteristic | Description |
|---|---|---|
| 1. B-cell ALL | The most common form (especially in children) | Arises from immature B lymphocytes; it typically responds well to standard chemotherapy. |
| 2. T-cell ALL | Often occurs in adolescents and young adults | Originates from T lymphocytes; can involve a mediastinal mass and may require more intensive therapy. |
| 3. Philadelphia Chromosome-Positive ALL (Ph+ ALL) | Contains BCR-ABL fusion gene | A more aggressive form is treated with Tyrosine Kinase Inhibitors (TKIs) like Imatinib or Dasatinib. |
| 4. Burkitt-type ALL | Very fast-growing variant | Shares features with Burkitt lymphoma; requires intensive, short-course chemotherapy. |
| 5. Mixed Phenotype Acute Leukemia (MPAL) | Displays features of both myeloid and lymphoid leukemia | Rare and requires customized treatment, often including bone marrow transplant. |
| 6. Relapsed/Refractory ALL | Disease returns after remission or doesn’t respond to treatment | May require novel therapies like CAR-T cell therapy or allogeneic stem cell transplant. |
Symptoms of Acute Lymphocytic Leukemia
Early detection of ALL can significantly improve treatment outcomes. The symptoms are often nonspecific and can resemble those of other illnesses, which can make early diagnosis challenging. Common symptoms include:
- Fever and Night Sweats: Unexplained fever and excessive sweating at night, often due to infections or the disease itself.
- Easy Bruising and Bleeding: Frequent nosebleeds, bleeding gums, or easy bruising as a result of low platelet counts.
- Bone and Joint Pain: Discomfort or pain in the bones and joints caused by the spread of leukemia cells to these areas.
- Swollen Lymph Nodes: Enlarged lymph nodes, especially in the neck, armpits, or groin, which can be painless or tender.
- Pale Skin: Anemia leading to pale skin, shortness of breath, and general weakness.
- Abdominal Pain: Swelling or pain due to the enlargement of the liver or spleen.
Diagnosis of Acute Lymphocytic Leukemia
- Blood Tests:
- Complete Blood Count (CBC): To check for low red blood cells (anemia), low platelets, and high white blood cell count (blasts).
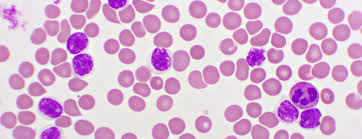
- Peripheral Blood Smear: To detect the presence of lymphoblasts.
- Bone Marrow Biopsy: Essential to confirm diagnosis and assess bone marrow involvement by lymphoblasts.
- Flow Cytometry: To identify specific markers on leukemia cells.
- Cytogenetic Analysis: To detect chromosomal abnormalities such as the Philadelphia chromosome (BCR-ABL fusion gene).
- Molecular Testing: To assess for specific genetic mutations, such as FLT3 and IKZF1.
- Lumbar Puncture (Cerebrospinal Fluid Test): To check for leukemia cells in the central nervous system (CNS) in high-risk cases.
Treatment Options for Acute Lymphocytic Leukemia
Induction Phase (4–6 weeks)
-
Combination chemotherapy (Vincristine, Prednisone, Daunorubicin, L-asparaginase)
-
CNS prophylaxis (intrathecal methotrexate)
Consolidation/Intensification Phase
-
High-dose methotrexate, cytarabine
-
Repeated cycles over 2–3 months
Maintenance Phase (2 years for children)
-
Daily 6-MP, weekly methotrexate, monthly vincristine
Targeted Therapy (if Ph+)
-
Tyrosine Kinase Inhibitors (Imatinib, Dasatinib)
Bone Marrow Transplant (if high-risk or relapsed ALL)
-
Especially for adults or those with minimal residual disease (MRD)
Cost and Stay in India
Comprehensive ALL treatment in India typically ranges from $9,000 to $40,000, depending on treatment phases (induction, consolidation, maintenance), targeted therapy for Ph+ ALL, and whether a bone marrow transplant is needed.
| Treatment Type | India (USD) | Turkey (USD) | USA (USD) |
|---|---|---|---|
| Diagnostic Tests (CBC, Bone Marrow, Genetics) | $300 – $800 | $1,000 – $2,000 | $5,000 – $10,000 |
| Induction Chemotherapy (4–6 weeks) | $4,000 – $6,000 | $8,000 – $12,000 | $40,000 – $60,000 |
| CNS Prophylaxis + Consolidation Therapy | $3,000 – $5,000 | $6,000 – $10,000 | $30,000 – $50,000 |
| Maintenance Therapy (2 years) | $2,000 – $3,500 | $5,000 – $7,000 | $25,000 – $40,000 |
| Targeted Therapy (TKIs – monthly) | $800 – $1,500 | $2,500 – $4,000 | $8,000 – $15,000 |
| Blood Transfusion (per unit) | $80 – $120 | $150 – $300 | $500 – $800 |
| Bone Marrow Transplant (if required) | $25,000 – $35,000 | $40,000 – $60,000 | $400,000 – $500,000 |
| Hospital Stay (4–6 weeks inpatient) | $2,000 – $3,000 | $5,000 – $7,000 | $30,000 – $50,000 |
Recovery Period for Acute Lymphoblastic Leukemia (ALL)
| Treatment Phase | Estimated Recovery Duration | Details |
|---|---|---|
| Induction Chemotherapy | 4–6 weeks (in hospital) | Initial phase to induce remission; patient closely monitored for infections |
| Consolidation Therapy | 2–3 months (with periodic hospital visits) | Destroys residual cancer cells and prevents relapse |
| Maintenance Therapy | Ongoing for up to 2 years (especially in children) | Oral chemotherapy; patients usually resume their daily routine with precautions |
| Bone Marrow Transplant | 3–4 weeks inpatient + 6–12 months full immune recovery | Required for high-risk or relapsed cases; needs long-term follow-up |
| Immune System Normalization | Up to 12 months after treatment ends | Full immune rebuilding with precautions, vaccines may be re-administered |
| Return to Normal Life | 6 months (children), 9–12 months (adults), varies by response | Most patients resume school/work gradually with periodic monitoring |
Regular Follow-Ups:
-
Blood counts, bone marrow checks, MRD (Minimal Residual Disease) monitoring
-
Follow-up schedule: Weekly (early), then monthly → quarterly over 2–3 years
Frequently Asked Questions
Chemotherapy uses drugs to kill cancer cells or stop them from growing. In ALL, it’s usually given in phases: induction, consolidation (or intensification), and maintenance.
The induction phase is the first phase of chemotherapy aimed at killing as many leukemia cells as possible to achieve remission.
The consolidation phase, also known as intensification, involves more intensive chemotherapy to eliminate any remaining leukemia cells.
Maintenance therapy involves lower doses of chemotherapy over a longer period to prevent the cancer from returning.
Yes, radiation therapy is sometimes used in ALL to target leukemia cells in the brain or other areas if the cancer has spread.
A stem cell transplant involves replacing diseased bone marrow with healthy stem cells from a donor. It is often used for patients with high-risk ALL or those who relapse.