Autologous vs Allogeneic Transplant: Which Is Right for You?
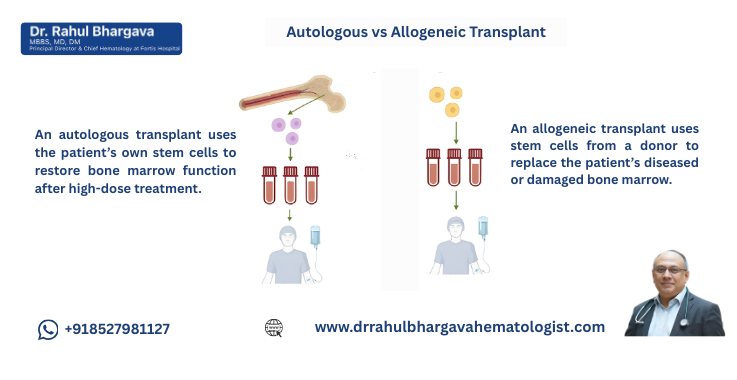
Table of Contents
Modern medicine has made it possible to treat many blood cancers and immune disorders with remarkable precision. One of the most life-changing treatment options available today is stem cell transplantation, commonly known as bone marrow transplant (BMT). If you are exploring BMT for yourself or a loved one, you have likely come across two major types:
Both approaches have helped millions of patients worldwide, but they work very differently. Understanding these differences is essential because the right type of transplant depends on your disease, health condition, and personal circumstances.
Understanding the Basics: What Exactly Is a Stem Cell Transplant?
Stem cell transplantation involves replacing unhealthy, damaged, or cancer-affected bone marrow with healthy stem cells. These stem cells grow into new blood cells; white cells, red cells, and platelets, helping your body recover from disease or intense treatments like chemotherapy.
Stem cells can come from:
- Your own body → Autologous transplant
- A donor’s body → Allogeneic transplant
Before we compare these two, let’s understand how the transplant process works.
What Happens Before the Stem Cell Transplant?
In most cases, doctors use high-dose chemotherapy or radiation to:
- Destroy diseased bone marrow
- Kill cancer cells
- Make space for new stem cells to grow
This is called conditioning therapy.
What Happens During the Stem Cell Transplant?
The healthy stem cells are infused into your bloodstream just like a blood transfusion. Over the next few weeks, these cells travel to the bone marrow and begin forming new, healthy blood cells—this is known as engraftment.
Why Are There Two Types of Stem Cell Transplant?
Because not every condition requires donor cells. Some diseases respond well when your own stem cells are used, while others need a complete immune reset using donor cells.
This is where the difference between autologous and allogeneic transplant becomes crucial.
Autologous Transplant (Auto-BMT)
Using Your Own Stem Cells: How It Works and Who It Helps
An autologous transplant uses stem cells that are collected from your own bone marrow or blood before you receive high-dose chemotherapy.
How Does an Autologous Transplant Work?
- Stem Cell Collection – Your stem cells are mobilized from bone marrow to blood and collected using a special machine.
- Freezing (Cryopreservation) – The collected cells are frozen and stored.
- High-Dose Chemotherapy – Doctors give strong chemo to destroy cancer cells.
- Stem Cell Infusion – Your frozen cells are re-infused to help your bone marrow recover.
This is called “rescue therapy” because your body uses its own cells to recover from aggressive cancer treatment.
Conditions Commonly Treated with Autologous Transplant
Auto-BMT is ideal for cancers where the problem lies mainly in the tumour cells and not in the bone marrow stem cells themselves.
These include:
Multiple Myeloma (most common use)
Autologous transplant is considered the standard of care for eligible myeloma patients because:
- It helps achieve deep remission
- It significantly extends survival
- It allows doctors to use powerful chemotherapy safely
Lymphomas (Hodgkin & Non-Hodgkin)
Auto-BMT is used when:
- Lymphoma relapses after initial treatment
- The patient does not respond fully to chemotherapy
- High-dose therapy is needed for better control
Other Conditions
Less common indications include:
- Testicular cancer
- Solid tumours requiring high-dose chemo
- Some autoimmune diseases (experimental)
Advantages of Autologous Transplant
Lower Risk of Complications
Because the body receives its own cells, the risk of immune rejection or graft-versus-host disease (GVHD) is minimal.
Faster Recovery
Engraftment usually happens within 10–14 days, and hospital stay is shorter than allogeneic transplant.
No Need for Donor Matching
You don’t need:
- A donor
- HLA matching
- Donor-related delays
This speeds up treatment significantly.
Lower Risk of Infection Long-Term
Immune system recovers faster as the cells are your own.
Limitations of Autologous Transplant
Not Suitable for All Diseases
If your disease affects bone marrow stem cells like leukemia, your own cells cannot be used.
Possibility of Relapse
Since autologous transplant does not provide a new immune system, it depends solely on chemotherapy to kill cancer. If cancer cells survive, relapse is possible.
Risk of Contamination
Sometimes, cancer cells can be mixed with the collected stem cells, though special filtering techniques reduce this risk.
Allogeneic Transplant (Allo-BMT)
Receiving Stem Cells From a Donor: A More Complex but Powerful Option
An allogeneic transplant uses stem cells donated by:
- A sibling
- A matched unrelated donor
- A half-matched family member (haploidentical)
- Umbilical cord blood
This makes it fundamentally different from an autologous transplant.
How Allogeneic Transplant Works?
-
Finding a Donor – Donor is matched through HLA typing.
-
Conditioning – High-dose chemotherapy or reduced-intensity conditioning suppresses diseased marrow.
- Stem Cell Infusion – Donor cells are infused into the patient.
- Engraftment & Immune Rebuilding – The donor immune system takes over and begins producing new blood cells.
Conditions Commonly Treated with Allogeneic Transplant
Allo-BMT is preferred when the disease is rooted in the bone marrow or immune system.
Leukemia (ALL, AML, CML)
Allogeneic transplant is often lifesaving because donor cells can destroy remaining cancer cells, a powerful effect called graft-versus-leukemia (GVL).
Aplastic Anemia
Here, marrow fails to produce any blood cells. Donor stem cells can completely restore bone marrow function.
Myelodysplastic Syndrome (MDS)
Allo-BMT is often the only curative option.
Genetic and Immune Disorders
Including:
- Thalassemia
- Sickle cell disease
- Severe combined immunodeficiency
- Metabolic disorders (rare)
Advantages of Allogeneic Transplant
Graft-Versus-Cancer Effect
The donor immune system actively fights residual cancer cells. This is the biggest advantage over an autologous transplant.
Curative Potential
For many diseases like leukemia and MDS, allogeneic transplant offers the only chance for cure.
Healthy Marrow Replacement
Diseased or faulty marrow is replaced by a healthy immune system.
Limitations and Risks of Allogeneic Transplant
Though powerful, allo-BMT comes with significant risks.
Graft-Versus-Host Disease (GVHD)
The donor immune cells may see your body as foreign and attack it.
GVHD can be:
- Acute (first 100 days)
- Chronic (long-term)
It may affect skin, liver, lungs, and gut.
Infection Risk
Because the immune system is suppressed, infections can be serious in the first year.
Finding a Donor Is Not Always Easy
Only 25–30% of patients have a fully matched sibling donor.
The rest need unrelated donors or half-matched family donors.
Higher Treatment Toxicity
Stronger side effects, longer hospital stay, and more intensive follow-up are common.
Key Differences Between Autologous and Allogeneic Transplant
|
Source of Stem Cells |
Your own |
Donor |
|
Main Use |
Myeloma, lymphoma |
Leukemia, MDS, aplastic anemia |
|
GVHD Risk |
Almost none |
Present (major risk) |
|
Immune Reset |
No |
Yes (new immune system) |
|
Relapse Risk |
Higher |
Lower due to GVL |
|
Donor Needed |
No |
Yes |
|
Hospital Stay |
Shorter |
Longer |
|
Mortality Risk |
Lower |
Higher |
|
Curative Potential |
Limited |
High |
Which Transplant Is Right for You? Factors Doctors Consider
Choosing between autologous and allogeneic transplant is a complex decision. Doctors evaluate multiple factors:
Your Disease Type
The most important factor.
- Myeloma → Autologous
- Lymphoma → Autologous (sometimes Allogeneic)
- Leukemia → Allogeneic
- Aplastic anemia → Allogeneic
- MDS → Allogeneic
Stage of Disease
What matters:
- Whether the cancer is in remission
- Whether prior treatments worked
- How aggressive the disease is
Age and Overall Health
Younger, healthier patients tolerate allogeneic transplant better.
Older patients or those with other illnesses may be better suited for autologous transplant.
Donor Availability
If a suitable donor isn’t found in time, an autologous transplant may become the most immediate and practical choice. For cancers where it’s medically appropriate, it allows treatment to proceed without unnecessary delay.
Previous Treatments
Treatments like high-dose chemotherapy, previous radiation, or existing organ problems can all affect whether a person is eligible for a transplant.
What Recovery Looks Like After Each Transplant?
Recovery After Autologous Transplant
-
Engraftment happens quickly, allowing the body to start producing healthy blood cells sooner.
-
The immune system usually recovers within a few weeks, so patients don’t need prolonged precautions.
- Long-term medications are fewer, since there’s no risk of graft-versus-host disease.
- Many patients return to normal activities within 1–3 months, depending on their health and recovery pace.
Recovery After Allogeneic Transplant
-
Engraftment usually takes 2–4 weeks as donor cells settle in and begin producing new blood cells.
-
The immune system may take 6 months to a year to rebuild, so patients must follow extra precautions.
- Regular GVHD monitoring is essential, since donor cells can sometimes react against the patient’s tissues.
- Recovery involves more medications and frequent hospital visits to prevent infections and monitor progress.
- Full recovery can take 1–2 years, depending on overall health and the body's ability to adapt.
Long-Term Outlook: Survival and Quality of Life
Autologous Transplant Outlook
-
Most patients enjoy a good quality of life after recovery.
-
High remission rates are seen, especially in myeloma and many lymphomas.
- Relapse is possible, but modern treatments make it increasingly manageable.
Allogeneic Transplant Outlook
-
Offers one of the highest rates of complete cure, especially in many leukemias.
-
Long-term survival is steadily improving with advanced supportive care and modern transplant methods.
- GVHD remains a risk, but newer treatments and preventive measures have greatly improved outcomes.
Common Myths and Misconceptions
Myth 1: My Stem Cells Can Become Cancerous Again
Truth: Collected stem cells undergo strict testing; chances of contamination are extremely low.
Myth 2: Donor Cells Always Cause Rejection
Truth: With careful HLA matching and modern medications, the risk of severe graft-versus-host disease (GVHD) is much lower than most people think.
Myth 3: Transplant Is the Last Resort
Truth: Transplants are often used early in treatment to give patients the best chance at long-term remission.
Myth 4: Only Relatives Can Donate
Truth: A family donor isn’t required—millions of unrelated donors worldwide can provide a match.
Emotional and Psychological Aspects
A bone marrow transplant is more than just a medical journey, it’s an emotional one too.
Patients often face:
- Fear of complications and the unknown during treatment
- Anxiety before the procedure and uncertainty about outcomes
- Social isolation while recovering in a protected environment
- Physical fatigue that can affect daily life
- Worry about relapse even after treatment
Having a strong support system through counseling, support groups, and family involvement can make a huge difference, helping patients cope better and improving overall recovery.
Final Decision: Which Is Right for You?
There is no universal answer. But here is a simple guide:
Autologous Transplant Is Right for You If:
-
You have multiple myeloma or lymphoma
-
You need high-dose chemotherapy rescue
- Your bone marrow stem cells are healthy
- You prefer lower risks and faster recovery
Allogeneic Transplant Is Right for You If:
-
Your disease originates in bone marrow
-
You have leukemia, MDS, aplastic anemia, or genetic disease
- You need a new immune system
- A matched donor is available
- You want the highest chance of cure despite higher risks
Both autologous and allogeneic transplants have revolutionized modern medicine. Autologous transplants are faster, safer, and very effective for controlling diseases like myeloma and lymphoma. Allogeneic transplants, on the other hand, are often the gold standard and sometimes the only curative option for conditions such as leukemia, MDS, and severe bone marrow failure.
The best way to determine which approach is right for you is through:
- A detailed evaluation
- Genetic and HLA testing
- Discussion with a transplant specialist
- Understanding your risks and goals
Every patient’s journey is unique, and the right transplant can provide renewed health, long-term remission, and hope for a better future.
Frequently Asked Questions
Autologous transplant uses your own stem cells.
Allogeneic transplant uses donor stem cells.
The biggest difference is that an autologous transplant does not give you a new immune system, whereas an allogeneic transplant does.
Autologous transplants are commonly used for:
- Multiple myeloma
- Hodgkin and Non-Hodgkin lymphoma
- Relapsed testicular cancer
- Certain solid tumors
This procedure is usually done when your own bone marrow is still healthy, allowing your stem cells to be collected and used for the transplant.
Allogeneic transplant is preferred for conditions where the bone marrow or the immune system is diseased:
- Acute leukemias (AML, ALL)
- Chronic leukemia (CML, advanced stages)
- Myelodysplastic syndrome
- Aplastic anemia
- Thalassemia, sickle cell disease
- Immune deficiency disorders
GVHD is a complication of allogeneic transplant where donor immune cells attack the patient’s body.
It can affect the skin, liver, gut, lungs, or eyes.
Autologous transplant does not cause GVHD.
Generally, yes.
Auto-BMT has:
- Lower risks
- Fewer complications
- Faster recovery
But its ability to cure disease is limited compared to allogeneic transplant.
Autologous transplants can help patients achieve long-lasting and deep remission, especially in multiple myeloma and lymphoma. However, they usually don’t provide a complete cure, since the patient’s own immune system remains unchanged.
Because donor cells create a new immune system that can attack cancer cells.
This is called the graft-versus-leukemia (GVL) effect.
Autologous: 1–3 months for functional recovery
Allogeneic: 6–12 months (sometimes up to 2 years) due to immune rebuilding
No. You need a donor only for an allogeneic transplant. Autologous transplant uses your own stem cells, so no donor is needed.
Options include:
- Matched unrelated donor (from registry)
- Haploidentical (half-matched) donor
- Umbilical cord blood transplant
Modern techniques allow almost everyone to find a suitable donor.
Autologous: 2–3 weeks
- Allogeneic: 3–5 weeks or longer depending on complications
No. They can come from:
- Peripheral blood (most common)
- Bone marrow
- Umbilical cord blood (for allogeneic only)
Yes. A fully matched sibling is the ideal donor. But worldwide registries provide millions of unrelated donors for those who don’t have a sibling match.