How to Increase Progression-Free Survival (PFS) in Cancer Treatment — A Complete Patient-Friendly Guide
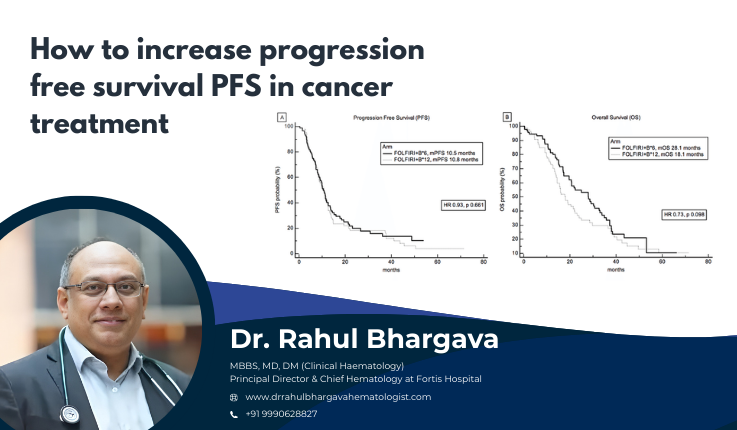
Table of Contents
Progression-Free Survival (PFS) is one of the most important measures in cancer care today. Improving PFS means helping patients live longer without the disease worsening — a key goal of modern cancer therapy.
In this detailed article, we will explain what PFS means, why it matters, and — most importantly — how clinicians and patients can work together to maximize PFS through state-of-the-art treatments, lifestyle strategies, supportive care, and emerging research.
Introduction: What Is Progression-Free Survival (PFS)?
Progression-Free Survival (PFS) is defined as the time from the start of treatment until the cancer gets worse or the patient dies from any cause. It is commonly used in clinical trials and real-world treatment outcomes to evaluate the effectiveness of a therapy.
Unlike Overall Survival (OS) — which measures the time until death from any cause — PFS focuses specifically on the length of time the disease is controlled without progression.
Why is PFS Important?
-
Earlier indicator of treatment effectiveness: PFS can show clinical benefit sooner than OS, especially in trials.
- Patient quality of life: Longer periods without disease progression often translate to better daily functioning and well-being.
Drug approval and clinical decisions: Many new cancer therapies are approved based on significant improvements in PFS.
Advanced and Tailored Treatment Approaches
Increasing PFS begins with choosing the most effective cancer therapy based on the tumor type, stage, genetic profile, and overall health of the patient.
Precision Medicine and Targeted Therapy
Precision medicine uses genomic profiling to tailor treatments based on a patient’s tumor characteristics. When targeted therapies block specific molecules needed for tumor growth, they can significantly delay progression.
Examples
- EGFR inhibitors like erlotinib improve PFS in non-small cell lung cancer versus chemotherapy alone.
- RET inhibitors are used for tumors with specific genetic mutations.
These personalized treatments often result in better tumor control and extended PFS.
Functional Drug Sensitivity Testing
Functional drug sensitivity testing (f-DST) is an emerging tool that tests a patient’s tumor cells against multiple drugs to find the most effective regimen.
How It Helps
- Selects the most promising chemotherapy or targeted combinations
- Reduces trial-and-error with ineffective drugs
- Potentially extends PFS with more precise initial therapy
Immunotherapy
Immunotherapy helps the body’s immune system recognize and destroy cancer cells. Several immunotherapies have dramatically improved PFS in cancers like melanoma, lung cancer, and bladder cancer.
Recent Advances
- Combination immunotherapy improved outcomes in bladder cancer, keeping many patients free from progression or death for longer time periods.
- CAR T-cell therapy extended PFS in some solid tumors in early trials, showcasing the potential of engineered immune cells.
Combination Therapies (Chemo + Targeted + Immunotherapy)
Many patients benefit when therapies are combined thoughtfully:
✔ Chemotherapy + targeted agents
✔ Immunotherapy + monoclonal antibodies
✔ Targeted therapy + hormone therapy
These combinations can be more effective in blocking multiple cancer survival pathways and delaying progression.
Maintenance and Sequential Therapy
Maintenance Therapy
Maintenance therapy refers to continued treatment after initial successful induction therapy to extend the time before progression.
Example:
In metastatic breast cancer, maintenance hormonal therapy after first-line chemotherapy has been shown to improve PFS.
Principle:
Keeping the cancer suppressed — even at a low dose — may delay relapse.
Sequential Therapy
Sequential therapy involves switching drugs or modalities at specific intervals or based on early signs of resistance. This keeps cancer from adapting and avoids early progression.
Surgical and Localized Interventions
Surgery for Limited Disease
For some patients with limited metastatic sites, surgical removal of tumors — followed by systemic therapy — may lead to better disease control and longer PFS.
Radiation Therapy Innovations
Advances such as:
- Stereotactic body radiotherapy (SBRT)
- Proton therapy
can target tumors more precisely and reduce the chance of regrowth.
Note:
Combining radiation with systemic therapy can sometimes yield added progression control.
Supportive Care and Symptom Management
Progression isn’t just about tumor growth — it’s also tied to how well patients tolerate therapy and manage side effects.
Managing Treatment Side Effects
Side effects from chemotherapy, targeted therapy, or immunotherapy (like fatigue, nausea, neuropathy) can limit treatment intensity and lead to treatment breaks — which can shorten PFS.
Effective supportive care includes:
- Anti-nausea medications
- Hydration and nutrition support
- Pain and symptom control
- Bone health management
Improved tolerance allows patients to stay on therapy longer, which can improve PFS.
Psychological and Emotional Support
Patients who feel supported and informed are more likely to adhere to treatment plans and maintain a healthier lifestyle, indirectly contributing to better outcomes.
Lifestyle, Diet, and Wellness
Although not a substitute for medical therapy, lifestyle choices can influence overall health and possibly impact disease progression.
Nutrition
A balanced diet rich in antioxidants, lean proteins, and anti-inflammatory foods supports immune function during therapy.
Stress Reduction
Stress hormones can interfere with immune response. Techniques such as mindfulness, yoga, or counseling help patients stay mentally strong.
Sleep and Circadian Rhythms
Emerging research suggests that the timing of chemotherapy or immunotherapy may influence outcomes because of circadian rhythms. Early-day treatment might be more effective in certain cancers.
Regular Monitoring and Early Detection of Progression
Imaging and Biomarkers
Frequent scans (MRI, PET, CT) and blood tests can detect subtle progression early.
Why It Matters:
Early detection of progression allows oncologists to modify or escalate therapy sooner, which may extend the next period of PFS.
Liquid Biopsies and Molecular Monitoring
Liquid biopsies — testing circulating tumor DNA (ctDNA) — are increasingly used to detect early relapse before it shows on imaging.
Clinical Trials and Emerging Research
Joining clinical trials can give patients access to the latest therapies that may improve PFS beyond standard care.
Innovative Trial Designs
Adaptive and early-endpoint focused trial designs — such as those using advanced analytics — aim to identify effective therapies faster and more reliably.
Personalizing PFS Goals with Your Oncology Team
Every patient’s situation is unique. Discussions about treatment goals — including PFS — should be personalized based on:
- Cancer subtype and stage
- Treatment history
- Overall health
- Patient preferences
The aim is not just to increase PFS but also to maximize quality of life during that time.
Conclusion: The Future of PFS in Cancer Care
Progression-Free Survival is more than a clinical metric — it reflects meaningful time for patients and families, free from disease worsening. With modern precision therapies, smart maintenance strategies, personalized treatment plans, supportive care, and lifestyle integration, PFS can be extended significantly for many cancers.
Cancer care is evolving rapidly, and ongoing research continues to unlock newer ways to keep cancer at bay for longer.
Frequently Asked Questions
Progression-Free Survival (PFS) is the length of time during and after treatment when a cancer patient lives without the disease growing, spreading, or worsening. It starts from the beginning of treatment (or randomization in trials) and ends when the cancer shows radiological or clinical signs of progression or when the patient dies, whichever comes first.
PFS is commonly used in cancer clinical trials and real-world oncology practice because it tells doctors how effective a treatment is at controlling the disease for a period of time.
PFS is important for multiple reasons:
-
It helps doctors understand how well a therapy works.
-
It provides a faster measure than overall survival (OS), especially in slower-growing cancers.
-
It helps in drug approvals, as many modern cancer therapies get approved based on PFS improvement.
-
Longer PFS often correlates with improved symptom control and better daily functioning.
For many patients, living longer without symptoms or tumor progression is a major quality-of-life benefit.
| Feature | PFS | OS |
|---|---|---|
| Measures | Time without disease progression or death | Time until death from any cause |
| Includes symptom progression? | Yes | No |
| Clinical significance | Earlier indicator of treatment benefit | Ultimate measure of survival |
| Used for approvals? | Very common | Less common because slower |
In some cancers, a treatment may improve PFS without improving OS, and vice-versa. Both are important metrics to understand treatment value.
Several factors influence PFS, such as:
-
Tumor biology (aggressive vs. slow-growing)
-
Cancer stage at diagnosis
-
Genetic mutations (e.g., EGFR, HER2, BRAF)
-
Choice of treatment modality
-
Patient age and overall health
-
Immune function
-
Response to therapy
-
Treatment adherence and tolerance
-
Lifestyle and nutritional factors
-
Supportive care availability
Because of these variables, PFS varies widely between individuals even with the same cancer type.
Several treatment categories are known to extend PFS depending on the cancer type:
-
Targeted Therapies: Drugs that target specific genetic mutations (e.g., EGFR inhibitors, RET inhibitors)
-
Immunotherapy: Checkpoint inhibitors (e.g., anti-PD-1, anti-CTLA-4), CAR-T therapy
-
Hormonal Therapy: Used in breast and prostate cancers
-
Chemotherapy: Standard backbone therapy for many cancers
-
Maintenance Therapy: Post-induction treatment to delay progression
-
Combination Therapy: Multi-drug regimens that block multiple cancer pathways
Advanced radiation, surgery, and ablative therapies may also contribute during specific disease stages.
