PFS Gains in Multiple Myeloma: What Patients Should Know
Table of Contents
Introduction
Multiple myeloma (MM) is a complex blood cancer that affects plasma cells — a type of white blood cell responsible for producing antibodies. Thanks to modern treatment advances, including targeted therapies, immunotherapy, and stem cell transplantation, patients are living longer and healthier lives than ever before. One of the most important measures used to evaluate the effectiveness of these treatments is Progression-Free Survival (PFS).
This blog will explain what PFS means, why it’s important, how it relates to overall survival and quality of life, what recent research shows about improvements in PFS, and what patients should consider when discussing treatment options with their healthcare providers.
What Is Progression-Free Survival (PFS)?
Progression-Free Survival, or PFS, is defined as the length of time during and after treatment that a patient lives with multiple myeloma without the disease getting worse. In other words, it’s the period from the start of a therapy until the cancer shows signs of progression or a patient dies from any cause.
Why Is PFS Measured?
In clinical trials and treatment evaluations, PFS helps researchers and clinicians understand how well a therapy controls cancer. Because PFS events (disease progression or death) occur sooner than long-term outcomes such as overall survival (OS), PFS allows for quicker evaluation of treatment benefits, especially in trials where waiting for long-term survival data can take years.
PFS vs Overall Survival (OS)
- PFS measures time until progression or death.
- OS measures time until death from any cause, regardless of disease progression.
While OS remains the most meaningful endpoint because it reflects actual survival duration, it takes longer to measure. Therefore, PFS often provides an earlier indicator of treatment efficacy and is widely used in research and regulatory decisions.
Why Does PFS Matter in Multiple Myeloma?
A Direct Measure of Disease Control
Multiple myeloma can vary widely in how it behaves: some patients experience stable disease for months or years, while others progress more quickly. PFS tells us how long a treatment is able to keep the cancer from worsening. That makes it incredibly valuable for patients and doctors who need to choose the most effective therapy.
PFS and Treatment Decisions
Improved PFS often suggests that a treatment regimen is keeping myeloma under control for longer, which can translate into longer periods of remission and fewer symptoms. Treatments that significantly increase PFS may be preferred options, particularly for patients aiming for an extended quality life.
PFS Is Accepted by Regulatory Agencies
Regulatory bodies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) often use PFS as a key primary endpoint in clinical trials leading to cancer drug approvals — including in multiple myeloma. PFS can accelerate access to promising therapies by showing clinical benefit earlier.
How Is PFS Calculated in Clinical Trials?
In research settings, clinicians track PFS using:
- Blood tests (e.g., myeloma protein levels, biomarker changes)
- Imaging studies
- Bone marrow tests
- Clinical assessments
Progression is typically defined as a significant increase in myeloma protein levels, new lesions, or clinical symptoms indicating disease worsening.
PFS as a Surrogate Endpoint
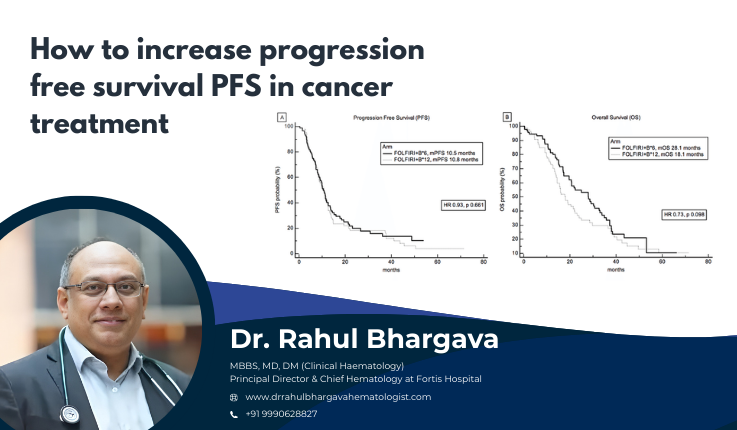
In multiple myeloma trials, PFS is considered a surrogate endpoint — meaning improvements in PFS usually predict improvements in overall survival and patient benefit, although this relationship can vary. Recent studies have shown a strong correlation between increments in PFS and improvements in OS in relapsed or refractory myeloma. For example, each 1-month increase in median PFS was associated with about a 1.7-month increase in OS in one comprehensive analysis.
What Does “PFS Gain” Really Mean?
When oncologists talk about PFS gain, they refer to how much longer a therapy can delay disease progression compared to another treatment or control group.
Examples of PFS Gains
-
A new therapy might increase median PFS from 18 months to 30 months compared to another regimen.
- A transplant combined with maintenance therapy may extend PFS significantly compared to drug therapy alone.
Recent randomized studies — including large phase 3 trials — have shown meaningful PFS improvements when modern combination therapies are introduced or when novel agents like monoclonal antibodies are added.
Which Treatments Deliver PFS Benefits?
There’s no single treatment for every patient, but many effective therapies aim to lengthen PFS in multiple myeloma. These include:
Combination Therapies
-
Proteasome inhibitors, immunomodulatory drugs, and steroids in combination.
- Newer regimens often include monoclonal antibodies like daratumumab or isatuximab.
Clinical trials like PERSEUS have shown improved PFS when daratumumab is added to the standard VRd protocol (bortezomib, lenalidomide, dexamethasone), with higher rates of deep and sustained responses.
Autologous Stem Cell Transplant (ASCT)
ASCT remains a key part of therapy for eligible patients. Studies like the DETERMINATION trial show that transplant can lead to a significant PFS benefit when added to induction and maintenance therapies, especially in younger or high-risk patients.
Maintenance Treatments
Maintenance therapy following initial treatment or transplant — especially with lenalidomide — has been shown to keep myeloma under control for longer, thereby increasing PFS.
Novel Agents and Targeted Therapies
Newer drugs targeting specific pathways or markers on myeloma cells continue to improve PFS in both newly diagnosed and relapsed populations.
PFS Gains and Quality of Life
While PFS measures disease control, patients naturally want to know how it affects everyday life. PFS gains often correlate with:
- Longer periods without disease symptoms
- Reduced need for hospitalizations
- Better energy and functioning
- Less frequent changes in therapy
However, side effects from treatment matter too. A therapy that extends PFS but causes significant toxicity may negatively impact a patient’s day-to-day life. That’s why PFS needs to be considered in the context of quality of life (QoL) — an essential part of treatment decision making.
How Patients Can Use PFS Information
Understanding PFS helps patients in several important ways:
Ask Informed Questions
Patients can ask their care team:
- “What did the studies show about PFS with this treatment?”
- “How does extending PFS translate into daily life benefits?”
- “What are the side effects compared to the PFS gain?”
Make Shared Decisions
PFS data can inform shared treatment decisions, helping align therapy choices with personal goals — whether that’s longer disease control, fewer side effects, or avoiding frequent clinic visits.
Understand Prognosis
PFS is one piece of the prognostic picture — alongside overall survival, response rates, and biomarkers like minimal residual disease (MRD) status.
Real-World Examples of PFS Improvements
Research shows large variations in PFS depending on the therapy used:
- Triple drug regimens plus transplant showed longer PFS than some older treatment combinations.
- Modern quadruplet therapies with monoclonal antibodies demonstrate statistically significant PFS gains over standard therapy in newly diagnosed patients.
- Maintenance therapies further improve PFS when used long-term.
These examples illustrate how advancing research and personalized treatment approaches are delivering measurable benefits in disease control.
Limitations and Considerations
While PFS is a powerful tool, it’s not perfect.
PFS Does Not Always Predict OS
Although often correlated, longer PFS doesn’t always translate into longer overall survival for every patient or every regimen. Some therapies extend PFS without showing a significant OS difference.
Side Effect Burden
A treatment that lengthens PFS but introduces significant toxicity may not be the best choice for everyone. Quality of life needs to be weighed carefully.
Individual Differences
PFS gains seen in clinical trials may differ in real-world settings due to patient variability, co-existing conditions, and differences in supportive care.
The Future of PFS in Multiple Myeloma
The future of myeloma treatment — and the role of PFS — is bright. Emerging research is exploring:
- Biomarkers that predict deeper responses and longer PFS
- New agents that target resistant disease
- Combinations designed for high-risk patients
Continued research may further refine how PFS is used to guide treatment decisions.
Conclusion
Progression-free survival (PFS) is a cornerstone endpoint in multiple myeloma care. It offers an early insight into how well a therapy controls disease progression, informs treatment decisions, and helps patients and clinicians evaluate options together.
As treatments evolve, PFS gains are expected to grow — giving patients longer periods of disease control and improved quality of life. However, PFS should always be considered alongside overall survival, side effects, and personal treatment goals. Patients empowered with knowledge about PFS are better prepared to navigate their care journey with confidence and clarity.
Frequently Asked Questions
PFS stands for Progression-Free Survival, which is the length of time during and after treatment that a patient lives with multiple myeloma without the disease getting worse. In simple terms, it measures how long a treatment keeps the cancer under control before it progresses. PFS is widely used in clinical trials to evaluate how effective a therapy is at stopping disease growth.
PFS is important because it tells doctors and patients how well a treatment delays cancer progression. Longer PFS often means:
-
Longer periods without symptoms
-
Fewer hospital visits
-
Improved quality of life
-
Reduced need for switching therapies
Since multiple myeloma is not fully curable for most patients, maintaining long disease control becomes a key treatment goal.
PFS and OS are both clinical endpoints, but they measure different things:
-
PFS measures time until the cancer progresses or the patient dies.
-
OS measures time until death from any cause.
While OS reflects total lifespan, it often takes many years to measure. PFS provides earlier evidence on whether a treatment is working.
Not always — but often, yes. Studies suggest that in many multiple myeloma treatments, improvements in PFS correlate with improvements in overall survival, especially in relapsed or refractory cases. However, PFS doesn’t guarantee longer life on its own because survival also depends on:
-
Subsequent treatments
-
Patient age and health
-
Disease aggressiveness
-
Response to future therapies
Doctors measure PFS through routine monitoring such as:
-
Blood tests (M-protein, light chains)
-
Bone marrow biopsy
-
Imaging (PET-CT, MRI)
-
Clinical symptoms
If tests show that the cancer is growing again, or the patient dies, it is considered a PFS event.